

AC was well tolerated and showed a low rate of complications, with the benefit of maximal tumour excision and a potentially better patient outcome. AC in selected patients is an effective, safe and practical procedure, which is accompanied with a short hospital and ICU length of stay. AC patients showed a significantly Nutlin-3a chiral web better neurological outcome, faster discharge times and an uneventful surgery. Implementation of the new anaesthesiological approach was successful, with a low operative morbidity and rate of anaesthesia complications, short surgery time, and well tolerance by the patients. 2 groups (eloquent cortex AC n = 511, non-eloquent cortex AC n = 99) To elucidate the outcomes and potential advantages associated with AC for supratentorial tumour resection, treated by one neurosurgeon. No To analyse the individual anaesthetic management, intraoperative complications and postoperative outcome of patients undergoing AC. The safety and effectiveness of AC in 25 patients should be described. To assess the safety and effectiveness of AC in comparison to GA for lesions close to the eloquent cortex. Description of a new anaesthesiological protocol and patient outcomes for the first patients undergoing AC surgery in this institution. AC group showed less PONV and pain postoperatively. AC provides adequate sedation, analgesia and a smooth wake-up during the period of neurological monitoring with stable haemodynamic and acceptable respiratory parameters compared to general anaesthesia. Blood pressure was lower in the AC group during application of head clamp pins and emergence and the AC group required less vasopressors intraoperatively. Temporary episodes of desaturation and hypercapnia occurred more often in the AC group. Procedure: preoperative fMRI.Tumours in eloquent brain areas, otherwise considered as inoperable. The patient would not get these sequences if they do not enroll in this study. These optional sequences are for research only. The investigators may also ask to perform optional sequences during the scan.
Some patients may only require fMRI or DTI. Most patients will require both fMRI and DTI. The investigators will only perform the test sequences that are necessary for mapping the tumor. These new techniques may give the doctor a better view of where the brain tumor is located relative to important parts of the brain.

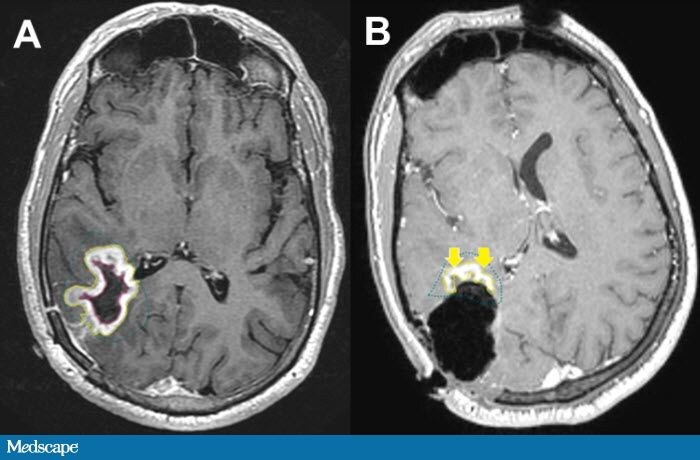
The investigators are studying new techniques for analyzing the MRI data. In other words, these tests are done as part of the best possible care even if they did not join this study. The scans are necessary stimulation for this protocol are part of the standard of care. The purpose of this study is to improve MRI mapping of the motor and language pathways in the brain. In patients who require stimulation as part of their standard of care, the investigators will compare the investigators imaging results with the stimulation results. Some patients may require stimulation during surgery to motor and language areas. Patients are scheduled to have imaging to help plan for possible surgery. These special MRI sequences are used to plan surgery. Patients usually get functional MRI (fMRI) or resting-state fMRI (rs-fMRI) for gray matter mapping and diffusion tensor imaging (DTI) or diffusion spectrum imaging (DSI) for white matter mapping. The investigators are studying the parts of the brain involved in motor and language. Avoiding these motor and language areas helps to prevent neurological deficits. These brain areas have roles in language or motor function. Some patients have brain tumors near important parts of the brain. Many patients with brain tumors require surgery. Why Should I Register and Submit Results?.


 0 kommentar(er)
0 kommentar(er)
